Just as selecting the right surrogacy partner and primary surrogacy professional is integral to a successful surrogacy experience, choosing the right surrogacy clinic is an important decision. Whether you call them “surrogacy clinics,” “fertility clinics,” or “IVF clinics,” intended parents and their gestational surrogate will all need to coordinate with this type of professional to complete the medical steps of the surrogacy process.
Here are four things you should always take into consideration when choosing a fertility clinic:
1. Location
Typically, both the gestational surrogate and the intended parents will work with the same fertility clinics individually in coordinating for certain appointments. The intended parents will work with a fertility clinic to create and prepare embryos, using gametes from the intended parents or donors. There may also be egg retrieval involved for the intended mother in some surrogacy situations.
Meanwhile, the surrogate will work with the intended parents’ fertility clinic to prepare for embryo transfer by taking the necessary fertility medications. She’ll need access to the clinic for scheduled testing, monitoring and more. For a surrogate, a conveniently located surrogacy clinic is a very important consideration, because she may be traveling back and forth to this location for appointments regularly until she’s pregnant.
Convenient and consistent access to a reputable surrogacy clinic isn’t always easy to come by, especially if you live in a rural area. Does a larger national clinic have a branch or an affiliated doctor at a local hospital near you? Can you realistically travel back and forth to a certain location? Location is something you’ll need to consider at the beginning of your surrogacy journey.
At Surrogate.com, you can find local surrogacy resources listed by state, including surrogacy clinics. Just click on your state, and go to the “Surrogacy Professionals” page listed there.
2. Cost
Surrogates will have the medical costs of their surrogacy journey covered, but finding a cost-effective fertility clinic that accepts your insurance is an important consideration when choosing a surrogacy clinic. Intended parents have probably invested a large sum of money toward having a child already, and they’ll need to budget their expenses at the fertility clinic carefully.
Your reproductive endocrinologist can help walk you through different IVF package options that a prospective clinic may offer, so you can choose what’s most cost-effective (and what’s most likely to be successful) based on your individual situation. That way, you’ll know you aren’t paying for anything you don’t need. We’ll also help intended parents and surrogates sort out their insurance policies, so everyone is covered as much as possible before you begin.
Of course, choosing a clinic exclusively on cost isn’t a good idea. The cheapest options aren’t always going to be the best options. You can always ask American Surrogacy for recommendations when you’re comparing costs of fertility clinics.
3. Success Rates
You’ll likely see intended parents and gestational surrogates discussing statistical success rates of fertility clinics in online forums. Another quick scan of these discussions, and you’ll also learn that some fertility clinics consistently accept patients with a lower (or higher) chance of success, which can skew their overall success rates.
There are organizations in the U.S. that track the reported success rates of surrogacy clinics, but you always have to take those reports with a grain of salt. Those numbers often don’t reflect the types of patients they work with, the cases they’re best qualified to handle, the experience of the providers, how many cases they take on, and other factors — so choosing a surrogacy clinic based solely on their statistical rate of success is never a good idea.
You can certainly take a clinic’s reported success rate into account when selecting the clinic you’d like to work with, but it shouldn’t be the only criteria you examine. You can view reports of IVF success rates for fertility clinics in the U.S. with these resources:
- Centers for Disease Control and Prevention (CDC)
- Society for Assisted Reproductive Technology (SART)
- Fertility Success Rates
4. Ability to Meet Your Needs
Finding a surrogacy clinic that offers the services you’ll need may take a little research. For example, you may need to check to make sure a particular clinic offers:
- Medical screening
- Cryopreservation
- Genetic screening of embryos
- In vitro fertilization (IVF)
- Connections to gamete banks
- Gamete retrieval
- Pregnancy testing for gestational surrogates
- And more
What you’re looking for in terms of services will depend on your individual surrogacy situation, but take note that not all fertility clinics or endocrinologists will offer the same range of services. Know what you’ll need, and what you can do without. Your American Surrogacy specialist can be a good voice of experience here.
Asking plenty of questions will be a good way to assess whether or not a surrogacy clinic is going to be the right fit for you and your surrogacy partner, so write down everything you can think of! Not sure what to ask? Your American Surrogacy specialist and former surrogates/intended parents who have been through this process themselves can give you suggestions to start with, so ask others for their advice. It’s a big decision, but you don’t have to make it alone.
Need some help finding the right surrogacy clinic? Ask an American Surrogacy specialist now by calling 1-800-875-BABY(2229).






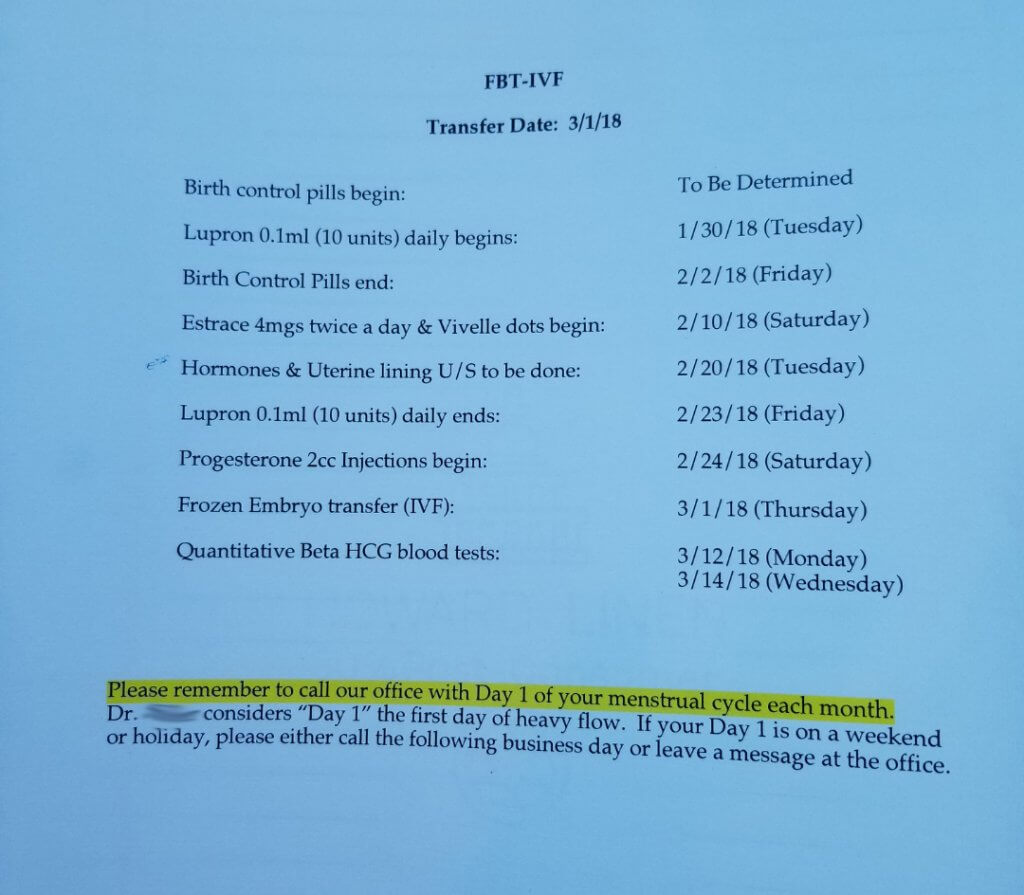
 I used a cheap Walmart drawer container to store my medications. I’m very type A, and it helped organize things. I was constantly getting new shipments and refilling it. I also downloaded blank calendar pages to fill in what medications I took each day. I marked them off as I took them. It was taped to my bathroom mirror.
I used a cheap Walmart drawer container to store my medications. I’m very type A, and it helped organize things. I was constantly getting new shipments and refilling it. I also downloaded blank calendar pages to fill in what medications I took each day. I marked them off as I took them. It was taped to my bathroom mirror.



