Having PCOS doesn't mean your family plans have to change. When polycystic ovary syndrome creates pregnancy complications or makes conception difficult, surrogacy provides an alternative route that sidesteps these medical challenges. Through gestational surrogacy, you can have your biological child while a surrogate manages the physical demands of pregnancy.
Get personalized guidance for your PCOS situation
You've probably explored multiple treatment options already, each with its own timeline and investment requirements. If you're considering surrogacy as a next step, you're looking at a well-established reproductive option.
Here's how surrogacy works specifically for people with PCOS, and why it often provides clearer outcomes than treatments that depend on overcoming your body's current limitations.
PCOS and Pregnancy: When Surrogacy Makes Medical Sense
PCOS affects roughly one in eight women of reproductive age, making it among the most common causes of fertility challenges.
The syndrome doesn't just influence ovulation patterns—it can affect pregnancy outcomes in ways that make carrying a baby medically complex. Most treatment plans start with lifestyle modifications, progress through ovulation drugs, IUI, then IVF.
These approaches work well for some people. For others, the underlying hormonal patterns create ongoing obstacles, or pregnancy risks become a significant concern. Gestational surrogacy offers a medical alternative: embryos created with your genetic material develop in someone whose reproductive system operates without PCOS-related complications.
Why PCOS Creates Pregnancy Challenges
PCOS presents differently across individuals, but certain patterns appear consistently. The condition typically involves elevated androgen levels, which disrupt normal ovulation cycles. Rather than releasing one mature egg monthly, ovaries often develop multiple partially-formed follicles that don't reach full maturity.
Insulin resistance frequently accompanies PCOS, creating additional complications. Elevated insulin affects hormone regulation and can compromise egg quality, making conception outcomes less predictable regardless of treatment approach.
Many people with PCOS also experience chronic low-grade inflammation, which research suggests may interfere with successful embryo implantation. These represent systemic physiological differences rather than correctable deficiencies.
Why IVF Success Rates Vary with PCOS
IVF outcomes for people with PCOS depend heavily on individual hormone profiles and treatment response patterns. Success rates range widely—some achieve pregnancy efficiently, while others experience repeated cycle failures despite good laboratory numbers. PCOS can make medication responses unpredictable, sometimes requiring higher stimulation doses that increase ovarian hyper stimulation risk.
Typical IVF challenges with PCOS include:
- Inconsistent medication response regardless of baseline hormone levels
- Variable egg quality even with good retrieval numbers
- Cycle modifications or cancellations due to unpredictable ovarian response
- Implantation difficulties that resist standard protocol adjustments
If you've completed several IVF cycles without achieving pregnancy, considering alternative approaches often makes practical sense.
How Surrogacy Addresses PCOS-Related Obstacles
Surrogacy circumvents the primary challenge PCOS creates: maintaining stable hormonal conditions throughout pregnancy. Working with someone whose reproductive system functions predictably removes many variables that complicate PCOS pregnancies.
Unlike IVF protocols that still require your body to support implantation and early pregnancy development, surrogacy transfers these biological functions to someone with demonstrated fertility success. This approach eliminates pregnancy complications that occur more frequently with PCOS, including gestational diabetes, pregnancy-induced hypertension, and preterm delivery risks.
Rather than managing these potential complications, you can concentrate on preparing for parenthood and building a working relationship with your surrogate. People often find this transition from medical uncertainty to collaborative planning particularly valuable after experiencing unpredictable treatment cycles.
Genetic Connection Through Surrogacy: Using Your Own Eggs
Genetic relationship concerns appear frequently in surrogacy discussions. Gestational surrogacy maintains complete biological connection—your child shares your genetic material, with the surrogate serving as the pregnancy carrier only. Embryo creation follows standard IVF protocols using your eggs and your partner's sperm.
When PCOS has significantly affected egg quality, using donor eggs remains an option while preserving genetic connection through your partner's contribution.
Many people also utilize frozen embryos from previous IVF attempts, which sometimes achieve better success rates since previous failures likely involved implantation or pregnancy maintenance rather than embryo quality issues.
PCOS Surrogacy Process: Medical Steps and Timeline
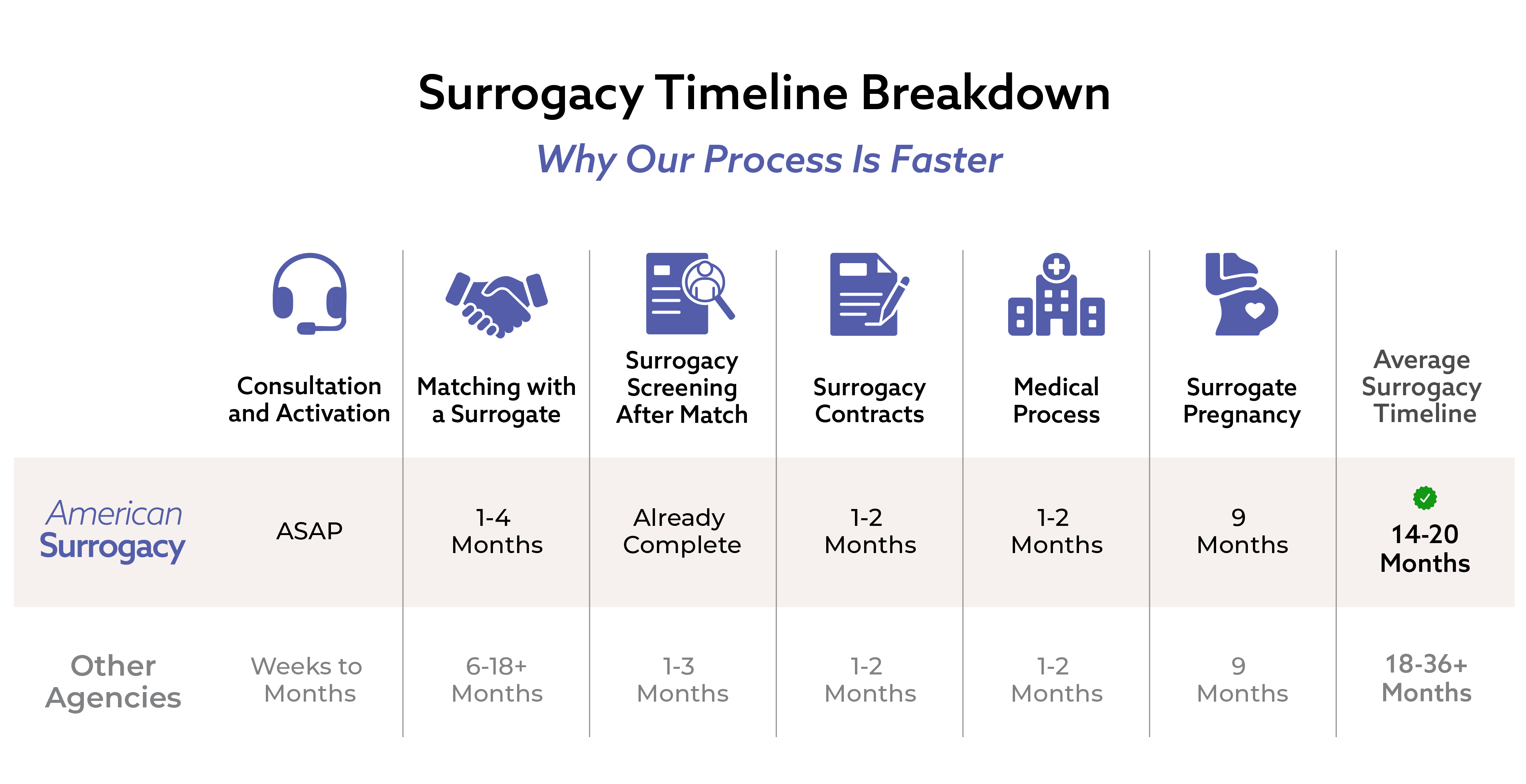
People with PCOS often appreciate surrogacy's structured timeline after dealing with unpredictable treatment cycles. Each phase operates on established protocols with realistic timeframes.
Step 1: Medical Consultation and Planning
We review your complete PCOS history and previous treatment records to develop an appropriate medical plan. This includes determining whether existing frozen embryos can be transferred or whether fresh embryo creation makes more sense.
Step 2: Surrogate Selection and Legal Framework
Connect with medically-cleared surrogates within 1 - 4 months months, based on compatibility factors including communication preferences, geographic considerations, and shared expectations. Legal contracts establish medical decision-making protocols and financial arrangements.
Step 3: Medical Coordination and Transfer
Synchronize medical protocols between your treatment and your surrogate's preparation cycle. Complete required health screenings and attend the embryo transfer procedure together.
Step 4: Pregnancy Management
Receive regular communication about prenatal appointments, test results, and pregnancy progression as your surrogate carries your developing baby.
Step 5: Delivery and Transition
Attend the birth with pre-established parental rights. Take your baby home directly from the hospital without additional legal processes.
This medical collaboration often provides more involvement and communication than people initially expect.
Surrogate Selection: Finding Medical Compatibility
Selecting an appropriate surrogate becomes particularly important after experiencing fertility challenges. Our evaluation process identifies women who understand the medical complexity involved when working with intended parents who have conditions like PCOS.
Every potential surrogate completes thorough medical examinations, psychological evaluations, and background investigations.
Our selection criteria prioritize:
- Documented pregnancy success with uncomplicated deliveries
- Medical literacy regarding surrogacy protocols and requirements
- Demonstrated reliability in medical and communication situations
- Strong interpersonal skills for collaborative relationships
- Stable support networks throughout pregnancy duration
Many surrogates have personal experience with fertility challenges—either directly or through close family members who underwent treatment. This background often creates better understanding and communication foundations.
Our selection process operates more efficiently than industry averages because we maintain an active pool of pre-qualified candidates, allowing you to move forward in 1 - 4 months months rather than extended waiting periods.

2 Months

1 Month

3 Weeks
Financial Analysis: Surrogacy Costs vs. Continued IVF
Cost considerations understandably concern couples who have invested significantly in previous treatments. When calculating accumulated expenses from multiple IVF cycles, medications, lost work time, and potential pregnancy complication management, surrogacy often represents comparable or better value relative to continued treatment attempts.
Our complete service packages range from $100,000 - $200,000+, including surrogate compensation, legal representation, medical expenses, and agency coordination.
Understanding What's Included and What's Additional
Base surrogacy packages typically include surrogate compensation, agency fees, legal contracts, psychological support, and standard medical procedures. Additional costs might include fertility clinic fees for embryo transfer, medications for cycle synchronization, and travel expenses if your surrogate lives in a different area.
Most agreements specify what happens financially if multiple embryo transfers are needed—often the surrogate compensation and agency fees remain the same, with only additional medical costs applying.
Multiple IVF cycles typically cost $40,000-$60,000 when including medications, monitoring appointments, and procedures. Factor in the physical recovery time and emotional investment of repeated attempts, and surrogacy's higher initial cost often produces better outcomes with reduced ongoing stress.
Consider this an investment in a treatment approach with higher probability of success, rather than continued attempts using methods that haven't produced desired results.
Financing Options After Previous Treatment Expenses
We recognize that considering surrogacy after existing treatment investments creates financial complexity. We've developed financing relationships specifically for families in this situation. Through Sunfish, you can access fertility-specific loans up to $300,000 with competitive rates and repayment terms designed for reproductive medicine expenses.
Additional financing approaches include:
- Employer fertility benefits (increasingly available across industries)
- Health savings account allocation for qualified medical expenses
- Retirement account loans or withdrawals for family-building purposes
- Fertility grants from established organizations like RESOLVE and Men Having Babies
- Family financing arrangements with flexible repayment structures
- Community fundraising platforms for broader support networks
Professional Support During PCOS Surrogacy
Transitioning from PCOS-related fertility challenges through surrogacy involves different emotional considerations for each individual. Access to professionals who understand both medical infertility and collaborative reproduction can significantly improve the experience.
Available support resources include:
- Fertility counseling specialists through our professional network
- RESOLVE support groups for PCOS and infertility (online and local chapters)
- PCOS Challenge organization for educational resources and community connections
- Online support communities including r/PCOS, r/surrogacy, and r/infertility
- Peer support groups for shared experience discussions
- Family counseling services for relationship support during treatment
Utilizing professional support represents good preparation for a significant life transition rather than indicating additional need or weakness.
Medical Decision-Making with PCOS
PCOS may have complicated your route to parenthood, but it doesn't determine your final destination. You've already demonstrated resilience managing fertility challenges—now you can apply that same determination to an approach that works with your medical situation rather than against it.
Our medical team has guided hundreds of individuals with fertility-related medical conditions through successful surrogacy processes. We understand both the frustration of treatments that don't achieve desired outcomes and the relief that comes with finding an approach that addresses your specific circumstances.
Ready to explore whether surrogacy fits your medical situation? Schedule a free consultation with our PCOS fertility specialists
Disclaimer: The information provided in this article is for educational and informational purposes only and is not intended as medical advice. American Surrogacy does not provide medical services and does not make clinical determinations regarding eligibility for fertility treatments or surrogacy. All medical evaluations and decisions should be made in partnership with licensed medical professionals.