Yes, you can have a biological child through surrogacy after any type of hysterectomy. Whether your surgery treated cancer, endometriosis, fibroids, or other conditions, gestational surrogacy allows you to become a parent using either your preserved eggs or donor eggs combined with your partner's sperm.
Hysterectomy removes your uterus but doesn't eliminate your path to genetic parenthood. This comprehensive guide explains how surrogacy works after partial, complete, and radical hysterectomy, details the egg retrieval and donor egg processes, and outlines why American Surrogacy has successfully helped hundreds of families navigate surrogacy after hysterectomy.
Genetic Connection Options Available After Hysterectomy
Your hysterectomy type determines which genetic connection options remain available:
- Partial hysterectomy (uterus removal only) preserves ovarian function, allowing egg retrieval and IVF to create embryos using both partners' genetic material.
- Complete hysterectomy (uterus and ovaries removed) eliminates your eggs but still enables genetic connection through your partner's sperm and donor eggs.
- Radical hysterectomy, typically performed for cervical or ovarian cancer, removes the most reproductive tissue but doesn't prevent surrogacy success. If oncology treatment allowed pre-surgery egg freezing, your preserved genetic material remains viable.
Without preserved eggs, donor eggs provide excellent outcomes with success rates matching those using intended parents' own eggs.
The emotional complexity of needing surrogacy after major surgery is completely normal. Grief over losing pregnancy capability can coexist with hope for parenthood. Both feelings deserve acknowledgment as you explore family-building options that honor your health journey while pursuing your parental goals.
The Complete Surrogacy Process Timeline after Hysterectomy
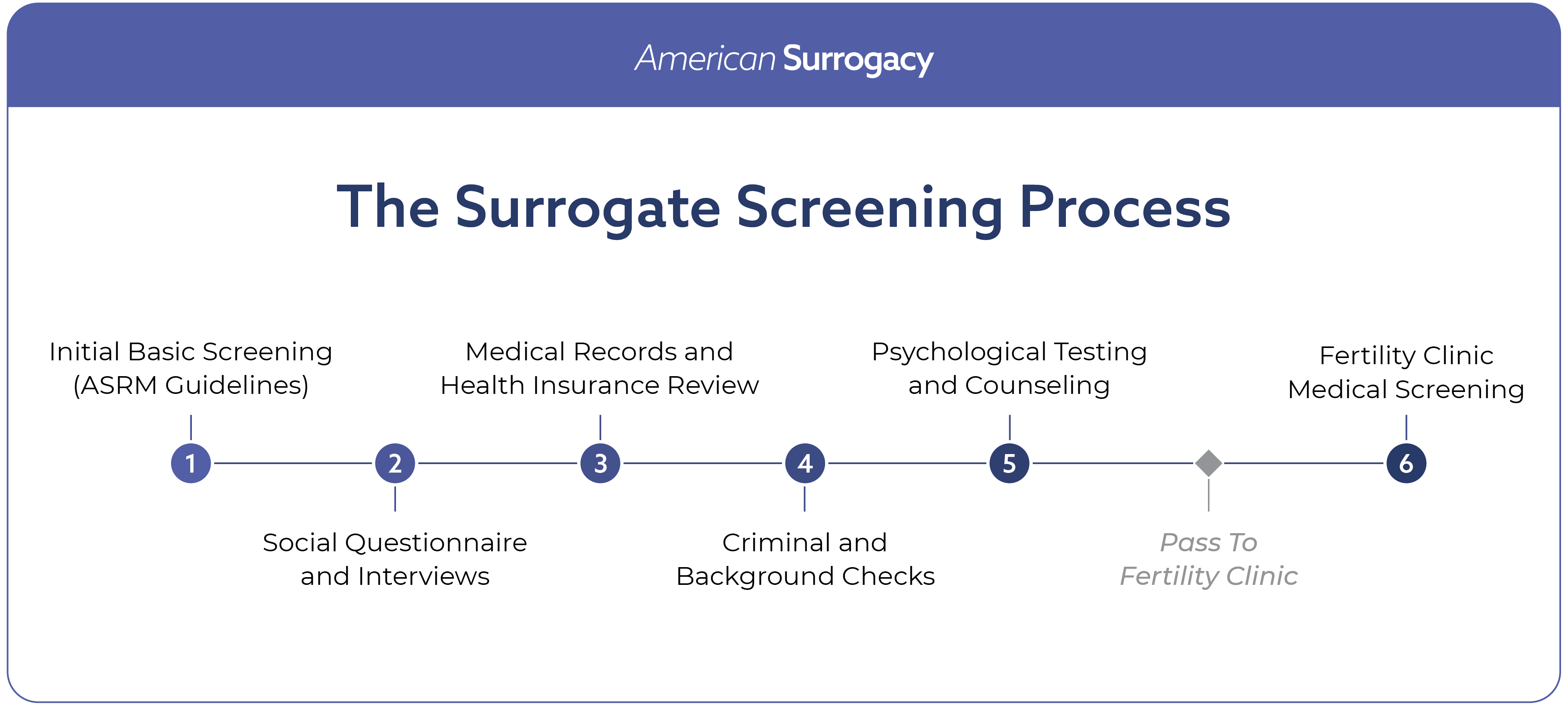
Surrogacy after hysterectomy follows a structured 12-18 month timeline designed to protect all parties while maximizing success potential. The process includes six distinct phases:
- Initial consultation and medical review - Comprehensive evaluation of your medical history and available options
- Surrogate matching and screening - Connection with pre-qualified gestational carriers who help families like yours
- Legal contract negotiation - Independent attorneys draft protective agreements for all parties
- Medical procedures and embryo transfer - IVF protocols and embryo transfer to surrogate
- Pregnancy monitoring and support - Coordinated prenatal care and communication management
Own Eggs vs. Donor Eggs for Surrogacy after Hysterectomy
Egg Retrieval Process after Partial Hysterectomy
Partial hysterectomy preserves ovarian function in 85% of cases, making egg retrieval possible when ovaries remain healthy. The retrieval process requires 10-14 days of fertility medications to stimulate multiple egg maturation, followed by a 30-minute outpatient procedure performed under sedation.
Retrieved eggs undergo immediate IVF fertilization with your partner's sperm. Resulting embryos can transfer fresh (3-5 days post-retrieval) or freeze for optimal timing coordination with your surrogate's cycle. Fresh transfers eliminate storage costs but require cycle synchronization, while frozen transfers offer scheduling flexibility and time for genetic testing.
Success rates using your own eggs after partial hysterectomy match those of standard IVF when ovarian function remains normal. Your fertility doctor evaluates hormone levels and antral follicle counts to predict retrieval success potential before beginning stimulation protocols.
Donor Egg Selection and Screening Requirements
Donor egg programs maintain extensive screening protocols ensuring optimal outcomes. Medical screening includes genetic testing for 300+ inherited conditions, infectious disease panels, hormone level assessments, and psychological evaluations. Donors undergo thorough family medical history review extending to grandparents when possible.
You select donors based on physical characteristics, educational background, personality traits, and genetic health profiles. Anonymous donors provide medical and personal information without identifying details, while known donors allow limited communication and ongoing relationships if desired.
Donor egg success rates exceed those using intended parents' eggs in many cases, particularly for women over 35 or those whose eggs were compromised by cancer treatments. Fresh donor cycles achieve pregnancy rates of 70-80% per transfer, while frozen donor eggs maintain 60-65% success rates.
Partial, Complete, and Radical Hysterectomy: Surrogacy Options
Partial Hysterectomy: Using Your Own Eggs for Surrogacy
Partial hysterectomy removes the uterus while preserving ovaries, maintaining natural hormone production and egg supply. This scenario offers the most direct genetic connection path, as your eggs combine with your partner's sperm to create embryos sharing both parents' DNA.
Timing flexibility benefits partial hysterectomy patients. Some women freeze eggs before surgery if hysterectomy is planned and fertility preservation is possible. Others pursue egg retrieval post-surgery when ovarian function remains stable and hormone levels support successful stimulation.
Recovery considerations affect timing. Most surgeons recommend waiting 3-6 months post-hysterectomy before beginning fertility treatments to ensure complete healing and hormone stabilization.
Complete Hysterectomy: Donor Egg Surrogacy Options
Complete hysterectomy removes both uterus and ovaries, eliminating natural egg production but preserving genetic connection through your partner's sperm. Donor eggs provide the female genetic component, creating embryos that carry your partner's genetic material and develop through gestational surrogacy.
Hormone replacement therapy often begins immediately after complete hysterectomy to manage surgical menopause symptoms. These hormones don't interfere with surrogacy protocols, and your surrogate's natural hormones support embryo development and pregnancy maintenance.
The donor egg selection process becomes particularly important for complete hysterectomy patients, as this represents your primary genetic connection option. Many intended parents find comfort in selecting donors who share meaningful characteristics or values.
Radical Hysterectomy: Post-Cancer Treatment Family Building
Radical hysterectomy typically follows cancer diagnoses requiring extensive reproductive tissue removal. Fertility preservation before cancer treatment offers the best genetic connection opportunities, but donor eggs provide excellent alternatives when preservation wasn't possible or successful.
Oncology clearance precedes surrogacy planning. Most oncologists require 1-2 years of cancer-free status before approving family-building activities, though timelines vary based on cancer type, staging, and treatment protocols.
Cancer survivors often experience heightened emotional complexity around family building, making professional counseling particularly valuable. Support groups for cancer survivors pursuing surrogacy provide peer connection and practical guidance from others with similar experiences.
Surrogate Matching Process for Intended Parents after Hysterectomy
All surrogates complete comprehensive medical evaluations including reproductive history review, current health assessment, and lifestyle factor analysis. Medical requirements include BMI between 19-32, absence of pregnancy complications in previous births, and current optimal health status without chronic conditions requiring medication management.
Psychological screening evaluates emotional stability, understanding of surrogate responsibilities, and support system adequacy. Surrogates must demonstrate clear understanding of the intended parent relationship and comfort with the medical and legal aspects of gestational surrogacy.
Lifestyle screening examines living situations, financial stability, and daily routines that support healthy pregnancy outcomes. This includes substance use history, support system availability, and time management capabilities for prenatal appointments and monitoring requirements.
Average Surrogate Matching Timeframes and Success Rates
American Surrogacy achieves average matching times of 1 - 4 months, significantly faster than industry standards of 18-24 months. Our pre-screening process ensures you're selecting from qualified candidates ready for immediate matching rather than waiting for screening completion after initial selection.
Matching success rates exceed 90% within six months for intended parents willing to consider multiple surrogate profiles. Geographic flexibility improves matching speed, as working with surrogates in different states expands available options without affecting legal or medical processes.
Re-matching occurs in less than 10% of cases, typically due to medical issues arising during screening or personal circumstance changes. Our matching team maintains backup options to minimize delays when re-matching becomes necessary.
Surrogacy Costs and Financial Planning After Hysterectomy
Surrogacy typically costs $100,000 - $200,000+ for complete programs including:
- Surrogate base compensation – 35% depending on location and experience
- Agency coordination fees – 21% for complete matching and support services
- Medical expenses – 12% covering prenatal care, delivery, and complications
- Legal representation – 6% for independent attorneys and contract drafting
- Miscellaneous expenses – travel, matching, insurance policies, screening, and other procedural costs vary by state, and make up the remainder of the average cost.
Compared to multiple IVF attempts, surrogacy often provides better value when considering cumulative costs and higher per-attempt success rates – especially when enrolled in a risk-protection plan, which lets you roll over or recover the majority of the funds you spent on surrogacy in the unlikely case of a disruption.
Surrogacy Financing Options and Payment Plans
We’ve recently partnered with Sunfish fertility financing, a firm that provides loans up to $200,000 with flexible repayment terms and competitive rates.
Multiple funding sources help make surrogacy financially accessible:
- Fertility grants and scholarships - Need-based funding for medically necessary surrogacy cases
- Employer fertility benefits - Growing number of companies covering surrogacy as standard healthcare benefit
- Personal medical loans - Specialized healthcare financing with favorable terms for fertility treatments
- Retirement fund access - 401(k) loans or hardship withdrawals for medical expenses without penalties
Our Limited Risk Program provides financial protection through refund guarantees if pregnancy doesn't result in live birth, reducing financial anxiety around this significant family investment.
Emotional Support Resources for Surrogacy after Hysterectomy
Specialized reproductive counselors understand the unique emotional challenges facing women who've lost pregnancy capability through medical necessity. Counseling addresses common concerns including loss of pregnancy experience, genetic connection anxieties, surrogate relationship boundaries, and fear of medical complications. Sessions help develop coping strategies for pregnancy milestones you're experiencing secondhand through your surrogate.
Digital communities provide 24/7 support from others who understand your specific situation. Reddit communities like r/hysterectomy and r/surrogacy offer practical advice, emotional support, and success story inspiration from women who've successfully built families after hysterectomy.
Professional facilitated support groups offer structured peer support with expert guidance. These groups often address specific challenges like managing anxiety during surrogate pregnancy or processing grief over reproductive loss.
Starting the Process for Surrogacy After Hysterectomy
Your consultation addresses five critical areas for informed decision-making:
- Medical history comprehensive review - Analysis of hysterectomy details, current health status, and fertility potential assessment
- Family-building pathway analysis - Detailed explanation of available options based on your specific surgical history
- Timeline and expectation management - Realistic projections for matching, medical procedures, and anticipated completion
- Financial planning and investment breakdown - Complete cost analysis with financing option exploration
- Support service introduction - Overview of counseling, coordination, and ongoing care resources available
Our team includes medical coordinators who understand the complexity of family building after reproductive surgery, matching specialists experienced with intended parents who've faced medical challenges, and support staff trained in the emotional aspects of surrogacy after hysterectomy.
The family you've been hoping for might be closer than you think. Schedule your consultation today to receive personalized guidance on your path forward. We'll address your medical concerns, explain your specific options, and help you take the first confident step toward the child who's waiting for you.
Frequently Asked Questions: Surrogacy After Hysterectomy
Can I have a baby through surrogacy after a hysterectomy? Yes, gestational surrogacy is possible after all hysterectomy types. Your options depend on whether ovaries were preserved, but even complete hysterectomy doesn't prevent genetic connection through your partner's sperm and donor eggs. Success rates match those of other surrogacy circumstances.
Do I need my own eggs for surrogacy success? No, donor eggs provide excellent outcomes equal to using your own eggs in many cases. When your eggs aren't available due to ovary removal or aren't viable due to medical treatments, donor eggs fertilized with your partner's sperm create healthy embryos for surrogacy.
How does surrogacy work after hysterectomy? The process creates embryos using either your retrieved eggs or donor eggs, fertilizes them with your partner's sperm, and transfers resulting embryos to a pre-screened gestational surrogate. The surrogate carries your genetic child to term while you maintain parental rights throughout pregnancy.
What are my alternatives to surrogacy after hysterectomy? Surrogacy provides the most direct path to biological parenthood when pregnancy isn't possible. Adoption offers another wonderful route to parenthood with different timelines and processes. Uterine transplant remains experimental with limited availability and success rates.
How long does surrogacy take after hysterectomy? Complete surrogacy typically spans 12-18 months from initial consultation to birth. Timeline factors include matching speed (average 3-4 months), legal contract completion (4-6 weeks), embryo creation if needed (2-3 months), and pregnancy duration (9 months).
What does surrogacy cost after hysterectomy? Total investment ranges $150,000-$200,000 covering all expenses: surrogate compensation, agency coordination, medical care, legal protection, and insurance management. Additional questions about costs and financing options can be addressed during your consultation to ensure complete financial understanding before beginning your journey.
Disclaimer: The information provided in this article is for educational and informational purposes only and is not intended as medical advice. American Surrogacy does not provide medical services and does not make clinical determinations regarding eligibility for fertility treatments or surrogacy. All medical evaluations and decisions should be made in partnership with licensed medical professionals.